TREATMENTS & PROCEDURES
SAY HELLO TO THE FUTURE OF SPINE CARE
TREATMENTS & PROCEDURESWe Recommend to Our Patients
General Spine
- Physical Therapy
- Medications
- Chiropractic Evaluation and Treatment
- Acupuncture
- Sacroiliac Joint Injection
- Sacroiliac Joint Minimally Invasive Fusion
- Medication Pain Management
- Weight loss program
- Smoking Cessation
Cervical Region
- Cervical Epidural Steroid Injection
- Cervical Facet Block and Radiofrequency Ablation
- Anterior Cervical Discectomy and Fusion
- Cervical Disc Replacement
Lumbar Region
- Lumbar epidural injection
- Lumbar facet injection and possible radiofrequency ablation
- Lumbar micro discectomy
- Lumbar laminectomy
- Lateral Lumbar Interbody Fusion (LLIF)
- Minimally Invasive Transforaminal Lumbar Interbody Fusion (MIS TLIF)
- Anterior Lumbar Interbody Fusion (ALIF)
- Robotic-assisted surgery
- Computer navigation
- Open lumbar fusion
GENERAL SPINE
- Physical Therapy
Overview:
Physical therapy is one of the most common and most effective treatments for neck and back pain. Our spine is completely surrounded by muscles, which move the core of the body and stabilize the spine. Those muscles can become strained and inflamed and go into spasm either due to injury (such as fall, heavy lifting, or a car accident) or overuse (physical labor, repetitive motions, obesity, or spine deformity). This can cause back or neck pain and stiffness without any structural problems inside the spinal column. Arthritis and inflammation inside the spine can also cause the surrounding muscles to become inflamed and go into spasm.
Description of the procedure:
Physical therapy uses various techniques to help with muscle spasms and inflammation as well as to prevent such problems from occurring in the future. Typically, the patient will have an initial evaluation where a licensed physical therapist will examine them and develop a specific treatment plan for their problem. The treatment typically starts with gentle stretching, massage, ultrasound, heat, ice, dry needling and other techniques to reduce pain, inflammation, and spasms. Once the patient is feeling better and is more functional, specific exercises to improve flexibility and muscle strength are added. Typical treatment course includes 2-3 visits to a physical therapy office per week for 6-8 weeks. Sometimes the treatment needs to be extended for longer periods of time. Patients are also directed to do certain exercises at home during the treatment and after the treatment has ended in order to maintain muscle strength and flexibility. This can prevent the symptoms from happening again in the future.
How it helps:
Physical therapy is very safe and effective. There are no scars or side effects, but it requires full cooperation of the patient with the treatment plan and the home exercise program. It is common to have a mild flareup of pain in the beginning of the treatment as the painful muscles are mobilized, but at the end of the treatment most patients feel much better and regain their full function.
- Pain Medications
Back and neck issues can cause a lot of pain, stiffness, and discomfort. Part of the treatment plan for this can be medications. There are many types of medications available for this problem. Different types of medications can address different causes and types of pain. It is best to talk to your doctor to determine which medication is best for you. It is very important to take medications ONLY as prescribed and direct any questions/concerns to your doctor.
- Chiropractic Evaluation and Treatment
Chiropractic manipulations can provide significant relief for back and neck pain. After an initial evaluation (which can include a series of x-rays), a chiropractor will develop a plan of treatment over a number of visits. Chiropractic treatment typically involves manipulation of the body, stretching, and other methods to address improper bone alignment and muscle spasms. Chiropractic manipulations have been around for thousands of years and can be effective for many problems, including back and neck pain.
- Acupuncture
Acupuncture treatments involve the placement of needles into various points on the skin. It is an ancient technique was developed thousands of years ago. It can be effective for numerous ailments including neck and back pain. Acupuncturists say that it works by re-aligning the bio-energy flow in the body that allows the body to heal itself. While the concept is not fully understood by modern science, multiple recent clinical studies have shown that it is effective in alleviating pain.
- Sacroiliac Joint Injection
Symptoms/conditions addressed:
Sacroiliac joint inflammation can cause significant low back and buttock pain, especially while sitting or walking.
Description of the procedure:
The problem is usually treated with physical therapy, medications, and activity modifications. If those treatments do not help, an injection of anti-inflammatory steroid and numbing medicine may be considered. This joint is deep, so it is very difficult to so the injection properly in a regular doctor’s office. For that reason, the patients are typically referred to a pain management physician or an interventional radiologist. The joint is then injected under x-ray guidance to make sure the tip of the needle is in the right place.
How it helps:
The medication decreases inflammation inside the joint and typically decreases the pain for about 3 months. If the injection only lasts for a short time, a radiofrequency ablation can be considered. During the ablation, the sensory nerves around the sacroiliac joint are destroyed by a small heating probe the size of a needle. This is also done by a pain management doctor. The ablation typically provides much longer lasting relief than the injection.
- Sacroiliac Joint Minimally Invasive Fusion
Symptoms/conditions addressed:
Sacroiliac joint fusion is usually offered for instability and degeneration that causes pain while sitting or walking.
Rationale:
Surgery is usually the “last resort” treatment for sacroiliac joint pain. It is usually offered only if other treatments have not helped or if the problem is so bad that only surgery can “fix” it. Traditional sacroiliac joint fusion technique involves a large incision over the buttock with a lot of muscle dissection to get to the joint. The procedure is effective to relieve the pain, but the recovery is long and painful due to the significant amount of muscle cutting involved. Recently, a minimally invasive method of sacroiliac joint fusion was developed.
Description of the procedure:
A small incision is made on a side of a buttock and 3 screws packed with bone graft are placed across the joint using x-ray guidance or computer navigation. This results in significant pain relief and much quicker recovery, because there is no muscle cutting involved. This procedure is done on an outpatient basis or with a one-night stay in the hospital for pain control. After the surgery, the patients will use crutches for 2 weeks to allow the soft tissues to heal and then physical therapy starts. The overall healing time before being able to return to full activity is usually 6-12 weeks.
How it helps:
The surgery is very successful, with over 90% of patients having significant and permanent relief of pain.
- Medication Pain Management
Low back and neck pain are usually treated with either conservative measures (non-opioid medications, physical therapy, injections, etc.) or with surgery. Sometimes the pain is quite severe, and the usual treatments either do not help or cannot be done due to a patient’s health or other factors. In such cases, stronger medications like opioids may be required to relieve pain and maintain function. Such medications are powerful but have significant potential side effects, can cause addiction, and may become less effective if taken for a long period of time. Surgeons typically only prescribe such medications for a short period of time to control severe pain right after surgery. If a longer duration of treatment or higher doses of medication are required, patients are typically referred to a pain management specialist. These doctors have specialized training in long-term pain management and can provide it more safely and effectively than most surgeons or primary care providers. Pain management specialists are also more familiar with how to provide adequate pain management for their patients while minimizing the risk of addiction and staying compliant with new opioid-prescribing laws and regulations.
- Weight Loss Program
Excessive weight can cause additional stress on discs, joints, and muscles around the spine, especially in the lower back. Multiple studies have shown that overweight patients are more likely to have low back pain. Over time the excessive weight can cause more “wear and tear” and faster development of arthritis in the spine. Losing the excessive weight has been shown (among multiple other health benefits) to decrease low back pain and improve function and physical ability. It is certainly not easy to do, but there are multiple methods and programs available that can be tailored to each patient’s abilities and lifestyle. The first step is to discuss weight loss with your primary care provider and decide which method will work best for you.
- Smoking Cessation
Smoking tobacco on a regular basis has been shown to be very detrimental to your health.
Nicotine and other substances found in cigarette smoke, chewing tobacco, electronic cigarettes, nicotine gums and patches can cause multiple forms of cancer, lung disease, heart disease, strokes and other problems.
Nicotine also causes accelerated degeneration of discs and joints in the spine, leading to early arthritis. This causes pain, stiffness, nerve compression, and disability. Nicotine also impairs the body’s healing ability and will slow down healing after any surgery, including spine surgery. This will increase the risk of surgical complications or failure of the surgery. In most cases, in order to maximize the benefits and minimize the risks of spine surgery, the operation will not be offered to a smoker until they quit.
Nicotine is a very addictive substance and quitting is never easy. There are multiple smoking cessation methods that have been shown to be effective. You can discuss with your primary care provider which methods works best for you. If a patient is able to fully quit, their overall health will improve and even the back pain can decrease. They would also have a much better chance of healing properly after spine surgery.
CERVICAL REGION
- Cervical Epidural Steroid Injection
Symptoms/conditions addressed:
Patients suffering from cervical stenosis and radiculopathy usually complain of arm and neck pain, arm numbness, and sometimes weakness.
Rationale:
Whenever nerves in the neck are compressed by a herniated disc or a degenerative bone spur, they also get inflamed. The injection of a steroid reduces this inflammation, which often alleviates the symptoms. The steroid medications used in these injections are very strong anti-inflammatory chemicals. These chemicals are synthetic forms of cortisol – a chemical our body produces naturally to reduce inflammation.
Description of the procedure:
The injection is usually done in the back of the neck by a specially trained pain management physician, a physiatrist, or an interventional radiologist. There are a lot of sensitive structures in that area, which is why the injection is done using x-rays. This way the physician can constantly monitor the location of the needle and inject the medication in the right spot. This procedure can be done either with local anesthesia or with sedation. It is usually done in a special procedure room with proper patient monitoring and x-ray equipment.
How it helps:
The injection is effective 70-80% of the time and the effects last on average 3 months. The injection does not “fix” the underlying problem of the disc herniation or the bone spur. Instead, it alleviates the symptoms and helps the patient be more functional for a period of time. During that time, the nerve can heal, or the disc herniation can get resorbed. This way even after the medication has “worn off” the symptoms do not come back. If the symptoms return or if there was only partial relief, this injection can be repeated. Typically, a patient can get 3 or 4 injections per year in the same spot.
Ultimately, if this injection does not help or only helps for a short period of time, a patient might consider surgery to achieve permanent relief of symptoms.
- Cervical Facet Block and Radiofrequency Ablation
Symptoms/conditions addressed:
When the joints are inflamed, they can become painful, causing neck pain and stiffness.
Rationale:
Cervical facet joints are small joints in the back of the neck that connect the cervical vertebrae together. These joints can be damaged and get inflamed due to trauma, such as a fall or a car accident. They can also degenerate and develop arthritis through the normal process of aging and wear and tear. Initial treatments include activity modifications, physical therapy, home exercises, and anti-inflammatory medications. If those treatments do not help, if the symptoms are severe, or if the symptoms are worsening, a facet injection (block) and radiofrequency ablation may be a good option.
Description of the Procedure:
First, the pain management doctor would need to determine if the neck pain is truly caused by the painful facet joint. Using a small needle, the joint and the sensory nerve near it are injected with long-acting numbing medication. Because there are many sensitive structures in the back of the neck, this injection is done using x-rays to make sure the tip of the needle goes in the right place. Once the injection is done, the patient will typically have relief of the neck pain and stiffness for 4-6 hours. This will confirm that the facet joint is the source of the pain.
The patient then returns for the second procedure. A small probe that looks like a needle is then placed on the painful joint, near the sensory nerve, using x-ray guidance. The probe then emits radiofrequency signal that gently heats the nerve and destroys it (the ablation).
How it helps:
Once the nerve is not functioning, the pain signals from the joint cannot get to the brain and the patient does not feel pain. The procedure effect lasts until the nerve regenerates, which typically takes 6-12 months. If the pain returns when the nerve grows back, the procedure can be repeated.
Ultimately, if this injection and ablation do not help or only help for a short period of time, a patient might consider surgery to achieve permanent relief of symptoms.
- Anterior Cervical Discectomy and Fusion
Symptoms/conditions addressed:
Arm pain, numbness and weakness, neck pain and stiffness.
Rationale:
Surgery is usually a “last resort” treatment for neck problems. It is usually offered only if other treatments have not helped or if the problem is so bad that only surgery can “fix” it. There are multiple reasons cervical fusion surgery may be needed. The most typical reasons are a cervical disc herniation that is compressing either the nerves or spinal cord, severe arthritis of the disc or facet joints, deformity (abnormal structure), and instability (vertebra are moving too much, causing pain or nerve compression).
Just like most spine surgeries, there is a lot of planning involved in arranging the anterior cervical discectomy and fusion. The patient needs medical clearance, preoperative tests, and the pre-certification from the insurance company. The length of surgery depends on how many levels need to be fused and on severity of the problem. In healthier patients this surgery may be done on an outpatient basis. Other patients may have the surgery done in a hospital and will go home after a 1 or 2 night stay.
The surgery is done through the front of the neck. Usually a horizontal incision is made on the left side, 1-2 inches long. The soft tissue structures are then moved out of the way and the spine is exposed. The disc is then removed, and all the nerves are decompressed. A spacer filled with bone graft material is then placed inside the disc space to restore proper anatomy and to keep the nerves decompressed. A small metal plate is then placed in front of the spacer to hold the bones together while the bone graft inside the spacer slowly turns into a bridge of bone connecting the two vertebrae together. This is the actual fusion. The spacer and the plate typically stay in the neck permanently and do not cause any problems.
After the surgery, the patients typically wear a brace for 2 weeks and then the brace is removed, and physical therapy is started.
How it helps:
The surgery helps with neck and arm pain, and it improves arm weakness and numbness. The success rate of this surgery is quite high, and most patients are back to normal function in 6-12 weeks. Because the soft tissues in the front of the neck get moved during the surgery, patients may develop some swallowing problems after the surgery. Such symptoms may be significant for several days, but then improve. Most patients will not have any problems swallowing in 6-12 weeks after the surgery.
- Cervical Disc Replacement
Symptoms/conditions addressed:
Arm pain, numbness and weakness, neck pain and stiffness.
Rationale:
Surgery is usually a “last resort” treatment for neck problems. It is usually offered only if other treatments have not helped or if the problem is so bad that only surgery can “fix” it. Cervical disc replacement surgery is usually offered to treat a herniated disc which is compressing nerves in the spine or to remove and replace degenerative disc causing neck pain.
Cervical disc replacement surgery is newer than traditional cervical fusion surgery. The main advantage of replacing the disc with moving parts (just like knee or hip replacement) is that the motion is preserved. This preserves full range of motion in the neck. It also does not place any significant stress on the discs above or below the operative level. This decreases the chance of those adjacent discs degenerating and needing treatment in the future. Recovery is usually quicker for disc replacement than fusion – there is no need for the brace and the patient is allowed to move their neck right away.
Cervical disc replacement surgery is technically more difficult and requires the spine surgeon to have separate training for this procedure.
Cervical disc replacement also does not fix all the problems with cervical spine. Sometimes fusion surgery will be required instead.Just like most spine surgeries, there is a lot of planning involved in arranging the cervical disc replacement. The patient needs medical clearance, preoperative tests, and the pre-certification from the insurance company. The length of surgery depends on how many levels need to be treated and on severity of the problem. In healthier patients this surgery may be done on an outpatient basis, other patients would have the surgery done in the hospital and go home after 1 or 2 night stay.
Description of the procedure:
The surgery is done through the front of the neck. There is typically a horizontal incision on the left side, 1-2 inches long. The soft tissue structures are then moved out of the way and the spine is exposed. The disc is then removed, and all the nerves are decompressed. A mobile disc replacement device is then inserted into the disc space and secured in place. The final position and motion of the implant is then checked with x-rays. The spacer stays in place permanently.
After the surgery the patients do not need a brace. Patients are allowed to move their neck right away. Ibuprofen is given after the surgery to help with pain and to prevent any bone material from growing into the implant. It is important for the patient to take ibuprofen as prescribed by the surgeon even if they do not have any pain, to prevent this bone formation which can interfere with the motion in the spacer. Physical therapy usually starts 2 weeks after the surgery.
How it helps:
The surgery helps with neck and arm pain as well as improves arm weakness and numbness. Success rate of this surgery is quite high, and most patients are back to normal function in 6-8 weeks. Because the soft tissues in the front of the neck get moved during the surgery, patients may develop some swallowing problems after the surgery. Such symptoms may be significant for several days, but then improve. Most patients will not have any problems swallowing in 4-8 weeks after the surgery.
LUMBAR REGION
- Lumbar Epidural Steroid Injection
Symptoms/conditions addressed:
Patients suffering from lumbar stenosis and radiculopathy usually complain of back and leg pain, leg numbness, and sometimes weakness.
The initial course of treatment involves activity modifications, physical therapy, home exercises, and anti-inflammatory medications. If those treatments do not help, if the symptoms are severe, or if the symptoms are worsening, a steroid injection may be a good option. The steroid medications used in these injections are very strong anti-inflammatory chemicals. These chemicals are synthetic forms of cortisol – a chemical our body produces naturally to reduce inflammation.
Rationale:
Whenever nerves in the lower back are compressed by a herniated disc or a degenerative bone spur, they also get inflamed. The injection of steroids reduces this inflammation, which alleviates the symptoms.
Description of the procedure:
The injection is usually done by a specifically trained pain management physician, a physiatrist, or an interventional radiologist. There are a lot of sensitive structures in that area, which is why the injection is done using x-rays, so that the physician can constantly monitor where the needle is and inject the medication in the right spot. This procedure can be done either with local anesthesia or with sedation. It is usually done in a special procedure room with proper patient monitoring and x-ray equipment.
How it helps:
The injection is effective 70-80% of the time and the effects last, on average, 3 months. The injection does not “fix” the underlying problem of the disc herniation or the bone spur. Instead, it alleviates the symptoms and helps the patient become more functional for a period of time. During that time, the nerve can heal, or the disc herniation can get resorbed. That way even after the medication has “worn off”, the symptoms do not come back. If the symptoms do come back or if there was only partial relief, this injection can be repeated. Typically, a patient can get 3 or 4 injections per year in the same spot.
Ultimately, if this injection does not help or only helps for a short period of time, a patient might consider surgery to achieve permanent relief of symptoms.
- Lumbar Facet Injection and Radiofrequency Ablation
Symptoms/conditions addressed:
Lumbar facet joints are small joints in the back of the lumbar spine that connect lumbar vertebra together. These joints can be damaged and get inflamed due to trauma, such as a fall or a car accident. They can also degenerate and develop arthritis (spondylosis) through the normal process of aging and wear and tear. When the joints are inflamed, they can become painful, causing low back pain and stiffness.
Rationale:
Initial treatments include activity modifications, physical therapy, home exercises, and anti-inflammatory medications. If those treatments do not help, if the symptoms are severe, or if the symptoms are worsening, a facet injection (block) and radiofrequency ablation may be a good option.
Description of the procedure:
First, the pain management doctor would need to determine if the back pain is truly caused by the painful facet joint. Using a small needle, the joint and the sensory nerve near it are injected with long-acting numbing medication. Because there are many sensitive structures in the back, this injection is done using x-rays to make sure the tip of the needle goes into the right place. Once the injection is done, the patient will typically have relief of the back pain and stiffness for 4-6 hours. This will confirm that the facet joint is the source of the pain.
The patient then returns for the second procedure. A small probe that looks like a needle is then placed on the painful joint, near the sensory nerve, using x-ray guidance. The probe then emits radiofrequency signal that gently heats the nerve and destroys it (the ablation).
How it helps:
Once the nerve is not functioning, the pain signals from the joint cannot get to the brain, so the patient does not feel pain. The procedure effect lasts until the nerve regenerates, which typically takes 6-12 months. If the pain returns when the nerve grows back, the procedure can be repeated.
Ultimately, if neither the injection or the ablation help, or only help for a short period of time, a patient might consider surgery to achieve permanent relief of symptoms.
- Lumbar Microdiscectomy
Symptoms/conditions addressed:
Lumbar disc herniation can cause significant inflammation and compression of nerves in the lumbar spine. This can lead to significant leg and back pain as well as leg weakness or numbness.
Rationale:
Most disc herniations can be treated successfully without surgery. Sometimes, however, the symptoms persist, worsen, or the disc herniation is so large that non-operative measures would not help. In such cases, surgical removal of the herniated disc to relieve the pressure on the nerves may be recommended.
Description of the procedure:
Lumbar microdiscectomy is a very common spine surgery. A small incision is made in the back, the lumbar muscles are moved out of the way and a small window is created in the bone in the back of the vertebra called lamina. For that reason, this procedure is often called “hemilaminotomy.” Once the bone overlying the herniated disc is removed, the nerves are gently pulled out of the way and the disc is exposed. The herniated portion of the disc is then removed to relieve the pressure off the nerve. The rest of the disc is left in place to continue its function. The wound is then closed. To visualize the small lumbar nerves, the surgeon usually uses an operative microscope or magnifying loupes, which is why the procedure is called “microdiscectomy”.
Just like most spine surgeries, there is a lot of planning involved in arranging the lumbar microdiscectomy. The patient needs medical clearance, preoperative tests, and the pre-certification from the insurance company. The length of surgery depends on how many levels need to be decompressed and on the severity of the problem. In general, this procedure is quick, complication rates are low, and many patients are be able to go home the same day. If the pain is too severe, or if the patients have underlying medical problems, they are kept overnight for observation. No brace is required after this surgery. The patients are typically directed to start physical therapy to regain their strength and flexibility 2 weeks after the surgery. Most patients can return to their normal activity in 6-8 weeks.
- Lumbar Laminectomy
Symptoms/conditions addressed:
Lumbar stenosis causes compression of the nerves in the lower back. This can cause significant low back and leg pain as well as leg weakness or numbness. In rare cases the stenosis is so severe that it can cause bowel or bladder incontinence (cauda equina syndrome). Most of the time lumbar stenosis can be treated successfully with non-operative treatments. When the symptoms persist, worsen, or if the stenosis is very severe surgery may be needed to remove the compression off the nerves.
Description of the procedure:
Lumbar lamina is the bony arch in the back of the spine that covers the nerves in the spinal canal. In order to visualize the nerves and decompress them, the lamina needs to be removed. The procedure to decompress the nerves in the lumbar spine under direct visualization is called laminectomy (or removal of the lamina). First, a small vertical incision is made in the back. The muscles are then gently removed off the lamina. The lamina is then removed, and the nerves are decompressed. Once all the nerves are free, the wound is closed. If several levels need to be decompressed, a surgical drain may be placed to remove any residual collection of blood. This drain is typically removed the next day.
Just like most spine surgeries, there is a lot of planning involved in arranging lumbar laminectomy. The patient needs medical clearance, preoperative tests, and the pre-certification from the insurance company. The length of surgery depends on how many levels need to be decompressed and on severity of the problem. In healthier patients this surgery may be done on an outpatient basis. Other patients would have the surgery done in the hospital and may go home after a 1 or 2 night stay. The complication rate is low. Most patients are ready to start physical therapy in 2 weeks after the surgery. No bracing is required. Most patients are back to normal function in 6-8 weeks after the surgery.
- Lateral Lumbar Interbody Fusion (LLIF or XLIF)
Symptoms/conditions addressed:
Fusion surgery is done to permanently connect, or fuse, two or more vertebrae in the spine together. The most common reasons to perform a fusion procedure are instability (bones are moving too much and cause pain and nerve compression), deformity (bones are improperly aligned, causing pain), and degeneration (severe wear and tear of the disc and joints in the spine causes pain every time the spine moves). Sometimes stenosis, or nerve compression, in the spine is so severe that the only way to properly decompress the nerves is to remove a significant amount of bone, which creates instability, so fusion is needed to “put everything back together.” It is a significant surgery and is only offered as “last resort” if non-operative treatments fail, or if the problem is so severe that only the surgery will help.
Description of the procedure:
There are multiple ways to perform a fusion procedure. The best option will be recommended by your surgeon and will depend on multiple factors including anatomy, the reason for the fusion, history of prior spine procedures, overall health, etc.
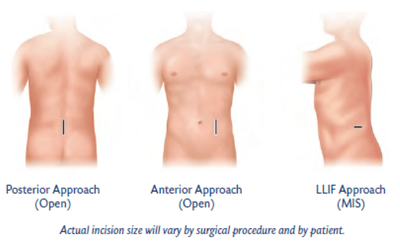
The minimally invasive advantage:
Minimally invasive spine fusions are new techniques that allow a surgeon to perform the procedure through a smaller incision with less soft tissue damage, while achieving the same successful fusion and nerve decompression as the traditional open techniques. Minimally invasive lumbar fusions have been shown to cause less pain, a lower chance of complications, less blood loss, quicker discharge from the hospital, and quicker overall recovery and return to function. With traditional open lumbar fusion, patients used to stay in the hospital for 3-5 days and had significant pain that required strong pain medications. The recovery typically took 6-12 months. The new minimally invasive surgical techniques allow the patients to go home after a one-night stay in the hospital, and in some cases even the same day. Most patients will not need any pain medications beyond 2-4 weeks after the procedure. The overall recovery is only 3-6 months.
Lateral lumbar interbody fusion is a minimally invasive surgical technique. It requires the surgeon to have specialized training and to utilize specialized instruments and monitoring. The patient is placed on their side, s small incision is made on the flank, and the disc between the vertebrae is removed. A spacer filled with bone graft material is then placed between the vertebrae where the disc used to be. The spacer re-aligns and stabilizes the vertebrae. The bone graft material slowly turns into a bony bridge that solidly and permanently fuses the two vertebrae together. Screws are then placed into the vertebrae through the back and are connected with rods to rigidly hold the bones together while the bone graft slowly turns into solid bone. Sometimes the LLIF is done with either computer navigation or robotic assistance, which makes the surgery safer and more efficient, with more precise placement of hardware.
Just like most spine surgeries, there is a lot of planning involved in arranging the LLIF. The patient needs medical clearance, preoperative tests, and the pre-certification from the insurance company. The length of surgery depends on how many levels need to be fused and on severity of the problem. Most patients can get out of bed and walk the day of the surgery and go home the next day. They usually do not need strong intravenous pain medications. Patients wear a lumbar brace for 6 weeks after the surgery to allow for initial healing. Physical therapy is then started and lasts about 6 weeks. Most patients are allowed to return to full physical function, sports, and manual labor work 3 months after the lateral lumbar interbody fusion.
- Minimally Invasive Transforaminal Lumbar Interbody Fusion (MIS TLIF)
Symptoms/conditions addressed:
Fusion surgery is done to permanently connect, or fuse, two or more vertebrae in the spine together. The most common reasons to perform a fusion procedure are instability (bones are moving too much and cause pain and nerve compression), deformity (bones are improperly aligned, causing pain), and degeneration (severe wear and tear of the disc and joints in the spine causes pain every time the spine moves). Sometimes stenosis, or nerve compression, in the spine is so severe that the only way to properly decompress the nerves is to remove a significant amount of bone, which creates instability, so fusion is needed to “put everything back together.” It is a significant surgery and is only offered as “last resort” if non-operative treatments fail, or if the problem is so severe that only the surgery will help.
Description of the procedure:
There are multiple ways to perform a fusion procedure. The best option will be recommended by your surgeon and will depend on multiple factors including anatomy, the reason for the fusion, history of prior spine procedures, overall health, etc.
The minimally invasive advantage:
Minimally invasive spine fusions are new techniques that allow a surgeon to perform the procedure through a smaller incision with less soft tissue damage, while achieving the same successful fusion and nerve decompression as the traditional open techniques. Minimally invasive lumbar fusions have been shown to cause less pain, lower chance of complications, less blood loss, quicker discharge from the hospital, and quicker overall recovery and return to function. With the traditional open lumbar fusion patients used to stay in the hospital for 3-5 days and had significant pain that required strong pain medications. The recovery typically took 6-12 months. The new minimally invasive surgical techniques allow the patients to go home after one-night stay in the hospital and in some cases even the same day. Most patients will not need any pain medications beyond 2-4 weeks after the procedure. The overall recovery is only 3-6 months.
In the MIS TLIF procedure two small incisions are usually made in the back. Gentle dissection is then made between muscle fibers down to the spine. The nerves are then decompressed, the disc is removed, and a spacer and bone graft material are placed inside the disc. The spacer realigns the bones and the bone graft material slowly turns into a solid bridge of bone permanently connecting the two vertebrae together. Screws are then placed into the vertebrae and connected with rods to rigidly hold the bones together while the bone graft slowly turns into solid bone. Sometimes MIS TLIF is done with either computer navigation or robotic assistance, which makes the surgery safer and more efficient, with more precise placement of hardware.
Just like most spine surgeries, there is a lot of planning involved in arranging the MIS TLIF. The patient needs medical clearance, preoperative tests, and the pre-certification from the insurance company. The length of surgery depends on how many levels need to be fused and on severity of the problem. Most patients can get out of bed and walk the day of the surgery and go home the next day. They usually do not need strong intravenous pain medications. Patients wear a lumbar brace for 6 weeks after the surgery to allow for initial healing. Physical therapy is then started, and it lasts about 6 weeks. Most patients are allowed to return to full physical function, sports, and manual labor work 3 months after the transforaminal lumbar interbody fusion.
- Anterior Lumbar Interbody fusion (ALIF)
Symptoms/conditions addressed:
Fusion surgery is done to permanently connect, or fuse, two or more vertebrae in the spine together. The most common reasons to perform a fusion procedure are instability (bones are moving too much and cause pain and nerve compression), deformity (bones are improperly aligned, causing pain), and degeneration (severe wear and tear of the disc and joints in the spine causes pain every time the spine moves). Sometimes stenosis, or nerve compression, in the spine is so severe that the only way to properly decompress the nerves is to remove a significant amount of bone, which creates instability, so fusion is needed to “put everything back together.” It is a significant surgery and is only offered as “last resort” if non-operative treatments fail, or if the problem is so severe that only the surgery will help.
Description of the procedure:
There are multiple ways to perform a fusion procedure. The best option will be recommended by your surgeon and will depend on multiple factors including anatomy, the reason for the fusion, history of prior spine procedures, overall health, etc.
Anterior lumbar interbody fusion is done through the front of the body. Because there are a lot of organs in front of the spine, this procedure is usually done with the help of a vascular or general surgeon. They help to safely move the intestines and large blood vessels out of the way. The spine surgeon then removes the disc between the two vertebrae and replaces it with a spacer filled with bone graft material. The spacer realigns and stabilizes the bones while the bone graft slowly turns into a permanent and solid bridge of bone to fuse the two vertebrae together. To hold the bones in place while the fusion is happening, a metal plate and screws can be applied to the front of the vertebrae or pedicle screws and rods can be inserted in the back. The general or vascular surgeon then checks to make sure there is no damage to the blood vessels and intestines and closes the wound.
Just like most spine surgeries, there is a lot of planning involved in arranging the ALIF. The patient needs medical clearance, preoperative tests, and the pre-certification from the insurance company. The length of surgery depends on how many levels need to be fused and on severity of the problem. Most patients are able to walk the day of the surgery and can go home the next day. The brace is worn for the first 6 weeks to allow for initial healing. After that, patients start physical therapy, which lasts another 6 weeks. Most patients are allowed to return to full function, sports, and physical activity 3 months after the surgery.
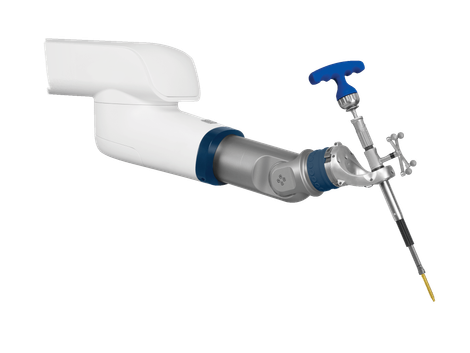
- Robot-Assisted Spine Surgery
Minimally invasive surgery of the spine can be quite complex. It is not easy to perform an operation through small incisions while minimizing complications and achieving surgical goals of nerve decompression, hardware placement, and bony fusion. A lot of times the hardware is placed using x-ray guidance or computer navigation. Spine surgery robots and navigation devices have been recently developed. They allow a surgeon to pre-plan the best possible placement of the hardware prior to surgery and then execute the plan precisely and efficiently using the robot during the operation. This minimizes chances of complications, especially improper screw placement. The robot uses computer navigation guidance which significantly reduces exposure of the patient to x-ray radiation. This new and amazing technology allows a surgeon to perform minimally invasive spine procedures through smaller incisions with high precision and efficiency.
- Computer Navigation:
Minimally invasive surgery of the spine can be quite complex. It is not easy to perform an operation through small incisions while minimizing complications and achieving surgical goals of nerve decompression, hardware placement, and bony fusion. A lot of times the hardware is placed using x-ray guidance or computer navigation. A CT scan of the spine can be done before or during surgery and the images are then loaded into the computer navigation system. That way the computer knows the exact 3D anatomy of the spine. The instruments used in navigated surgery have special trackers that allow the computer to know where they are in space relative to the spine. This way a surgeon can place instruments and hardware accurately into the spine through small incisions with no additional x-rays. This makes the operation more efficient and minimizes the amount of radiation exposure to the patient.
- Open Lumbar Fusion
Symptoms/conditions addressed:
Fusion surgery is done to permanently connect, or fuse, two or more vertebrae in the spine together. The most common reasons to perform a fusion procedure are instability (bones are moving too much and cause pain and nerve compression), deformity (bones are improperly aligned, causing pain), and degeneration (severe wear and tear of the disc and joints in the spine causes pain every time the spine moves). Sometimes stenosis, or nerve compression, in the spine is so severe that the only way to properly decompress the nerves is to remove a significant amount of bone, which creates instability, so fusion is needed to “put everything back together.” It is a significant surgery and is only offered as “last resort” if non-operative treatments fail, or if the problem is so severe that only the surgery will help.
Description of the procedures:
There are multiple ways to perform a fusion procedure. The best option will be recommended by your surgeon and will depend on multiple factors including anatomy, the reason for the fusion, history of prior spine procedures, overall health, etc. Minimally invasive techniques in spine surgery have been developed in the last 10-20 years. These techniques offer a lot of benefits, but they are more difficult to perform. Most of the minimally invasive spine surgery techniques assume that the spine anatomy is at least close to normal. Sometimes, a traditional open spine surgery can be a better option for the patient, especially if the anatomy is significantly altered, or if there is old hardware in the spine from prior surgery. Even with open techniques, care is always taken to minimize bleeding or damage to the surrounding tissues.
Just like most spine surgeries, there is a lot of planning involved in arranging open lumbar fusion. The patient needs medical clearance, preoperative tests, and the pre-certification from the insurance company. The length of surgery depends on how many levels need to be fused and on the severity of the problem. Open spine fusion typically requires a larger incision to properly visualize the nerves and bones. The nerves are decompressed, the hardware is placed to stabilize the bones, and bone graft is packed near the bones to achieve permanent fusion. The wound is then closed, and a surgical drain is usually placed to remove any residual collection of blood. This drain is typically removed the next day. The hospital stay is usually 3 days. Most patients would need to wear a brace for 6 weeks. This is followed by at least 6 weeks of physical therapy. Most patients can return to normal function, sports, and activity in 3-6 months.
SMALL INCISIONS,BIG IMPACT.
Learn how our minimally-invasive method of spine surgery can help you move past chronic back pain.
WHAT IS MINIMALLY INVASIVE SPINE SURGERY?
HOW DOES ROBOTIC SPINE SURGERY SYSTEM WORK?

Slide title
Write your caption hereButton
Slide title
Write your caption hereButton
Slide title
Write your caption hereButton
Slide title
Write your caption hereButton
Slide title
Write your caption hereButton
Slide title
Write your caption hereButton
Slide title
Write your caption hereButton
Slide title
Write your caption hereButton
Slide title
Write your caption hereButton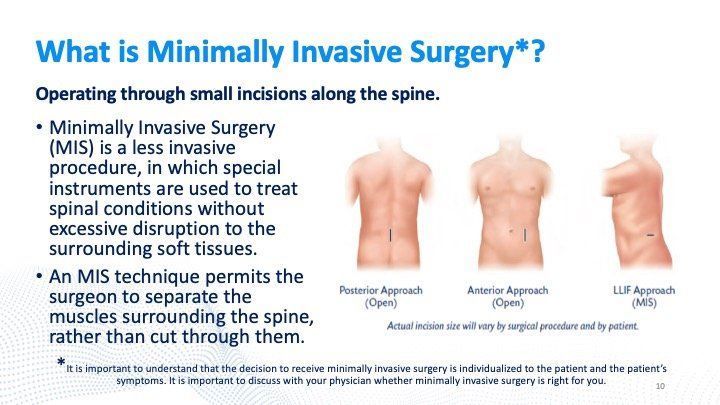
Slide title
Write your caption hereButton
Slide title
Write your caption hereButton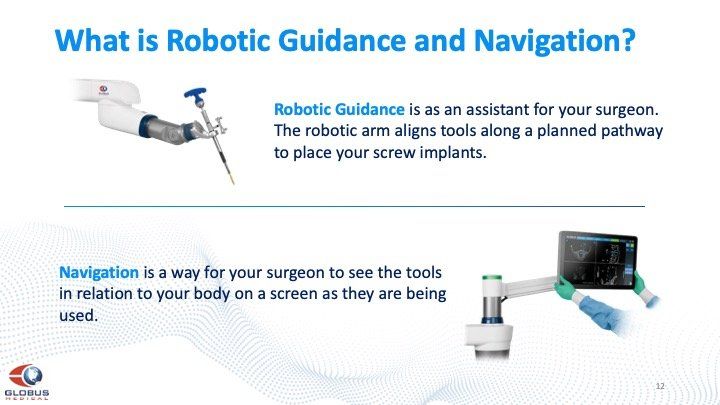
Slide title
Write your caption hereButton
Slide title
Write your caption hereButton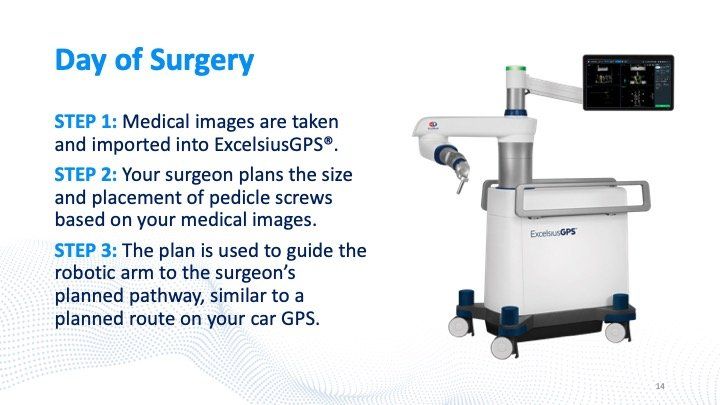
Slide title
Write your caption hereButton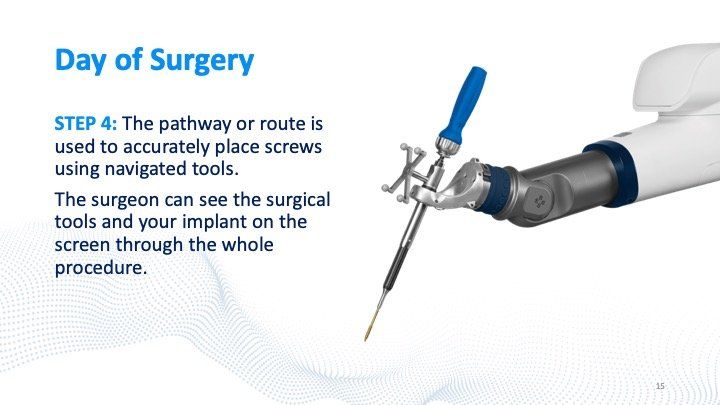
Slide title
Write your caption hereButton
Slide title
Write your caption hereButton